Pre-Lab Activity
Task 1
Before this week’s lab, find and watch a TED talk that provides some relevant information on the topic of cardiovascular disease. Send the link to the talk you watch to the subject coordinator by 8am on the Monday prior to the tutorial. The links will be compiled into a large list and posted on Canvas for the entire class to see.
Task 2
You will also need to conduct a brief review of two different types of activity logging devices (e.g., Fitbit, Garmin, Apple Watch, or relevant phone apps), including their main features and how they work.
The in class activities require the use of a health and fitness phone app that is able to record activity/step count. If you do not currently have one installed, please take the time to find a suitable app so that you can participate in class. The Health or Fitness apps are simple options for iOS users.
Write your notes from the talk you chose AND the activity logging devices you reviewed below.
If you are using the online lab manual, when you have completed the lab content and discussion questions for this week, print this webpage to PDF to save a copy on your device
All text entry boxes will clear if you leave or refresh this page
Lab Session - Part A
Questionnaires to Assess Functional Capacity, Barriers to Exercise, and Adherence to Exercise
Introduction
Exercise adherence is an important consideration in any program. There are many contributory elements to this complex issue, and while research continually builds around the topic, societal exercise habits about exercise participation are not improving. This tutorial content presents a range of questionnaires that provide non-physical methods to assess fitness, health and functional capacity along with some of the typically reported barriers to exercise.
The questionnaires are included for you to become familiar with by reading and completing them with the persona of an individual with a chronic condition. Please pick a range of symptoms that would typically be present in an individual with a cardiopulmonary, metabolic, musculoskeletal or neuromuscular condition.
Some of these questionnaires might be appropriate for you to include as part of the testing battery for your assignment.
Please also see the Appendices of this lab manual for some additional questionnaires that are relevant for a number of chronic diseases.
Questionnaires
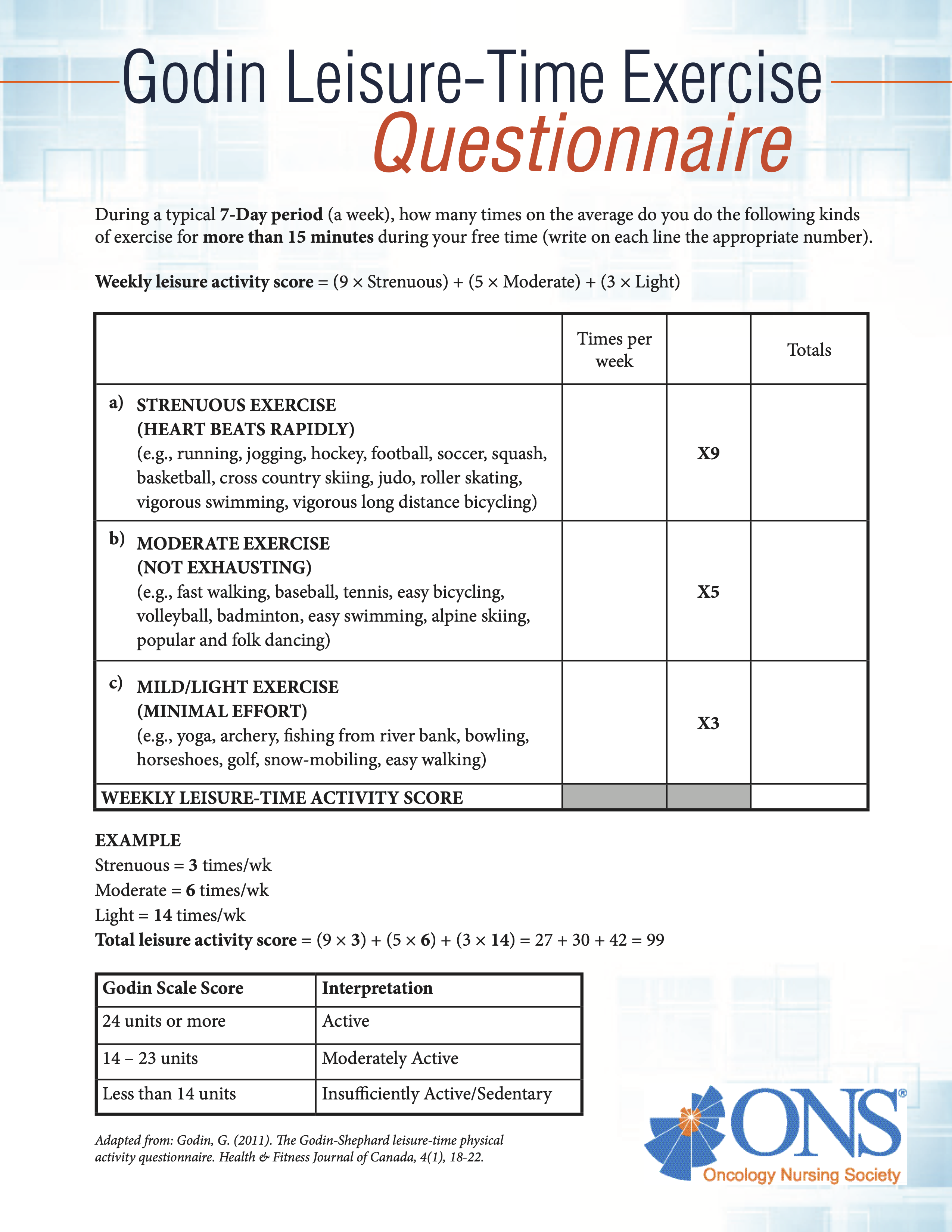
Godin Leisure-Time Exercise Questionnaire (LTEQ)
The LTEQ is designed to quantify voluntary exercise participation and provide a guide to current activity levels.
Screening Questionnaire for Cardiovascular Risk
This link provides a simple online cardiovascular disease risk assessment tool developed by the Heart Foundation in association with the Australian Chronic Disease Prevention Alliance.
The site also provides useful guidelines and resources for health professionals and the general public.
Lab Question 1
| Are questionnaires such as this valuable to the general population? List some positive and negative aspects of undertaking such a quiz below | |
| Positives: | |
| Negatives: | |
While completing the remaining lab activities, put yourself in the shoes of an individual with a chronic disease
Duke Activity Status Index (DASI)
The Duke Activity Status Index is a self-administered questionnaire that measures a patient’s functional capacity. It can be used to estimate a patient’s peak oxygen uptake. Please note that this test is for the non-healthy population, therefore, results for the healthy population will be under-estimated.
Read each question in the Activity column and select the value corresponding to your response in the Yes/No columns.
Once complete, sum the values circled and write it in the Total row. You can then use this number to calculate estimated peak oxygen uptake (VO2peak).
| Item | Activity | Yes | No |
|---|---|---|---|
| 1 | Can you take care of yourself (eating dressing bathing or using the toilet)? | 2.75 | 0 |
| 2 | Can you walk indoors such as around your house? | 1.75 | 0 |
| 3 | Can you walk a block or two on level ground? | 2.75 | 0 |
| 4 | Can you climb a flight of stairs or walk up a hill? | 5.50 | 0 |
| 5 | Can you run a short distance? | 8.00 | 0 |
| 6 | Can you do light work around the house like dusting or washing dishes? | 2.70 | 0 |
| 7 | Can you do moderate work around the house like vacuuming sweeping floors or carrying in groceries? | 3.50 | 0 |
| 8 | Can you do heavy work around the house like scrubbing floors or lifting and moving heavy furniture? | 8.00 | 0 |
| 9 | Can you do yardwork like raking leaves weeding or pushing a power mower? | 4.50 | 0 |
| 10 | Can you have sexual relations? | 5.25 | 0 |
| 11 | Can you participate in moderate recreational activities like golf bowling dancing doubles tennis or throwing a baseball or football? | 6.00 | 0 |
| 12 | Can you participate in strenuous sports like swimming singles tennis football basketball or skiing? | 7.50 | 0 |
| Total | |||
Estimated VO2peak (ml/kg/min) = 0.43 × DASI Score + 9.6 =
|
|||
Lab Question 2
| What are some limitations to the use of the DASI? |
The Activities-Specific Balance Confidence (ABC) Scale
For each of the activities below, use the number line and associated descriptors to rate your confidence that you will not lose your balance or become unsteady (Powell & Myers, 1995).
If you do not currently do the activity in question, try to imagine how confident you would be if you had to do the activity. If you normally use a walking aid to do the activity or hold onto someone, rate your confidence as if you were using these supports.
| 0 | 10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100 |
|---|---|---|---|---|---|---|---|---|---|---|
| Cannot do at all | Certain can do | |||||||||
| How confident are you that you will not lose your balance or become unsteady when you: | |
|---|---|
| Activity | Confidence |
| Walk around the house | |
| Walk up and down the stairs | |
| Bend over and pick up a slipper from the floor | |
| Reach for a small can off a shelf at eye level | |
| Stand on your tiptoes and reach for something | |
| Stand on a chair to reach for something | |
| Sweep the floor | |
| Walk outside to a nearby car | |
| Get in and out of a car | |
| Walk across a parking lot | |
| Walk up and down a ramp | |
| Walk in a crowded mall where people rapidly walk past you | |
| Are bumped into by people as you walk through the mall | |
| Use an escalator holding the rail | |
| Use an escalator not holding the rail | |
| Walk outside on wet sidewalks | |
| Total | |
Self-Efficacy for Exercise (SEE) Scale
This scale is a self-report of exercise self-efficacy (Resnick & Jenkins, 2000). There are 9 items to consider, with the total score is calculated by summing the responses to each question. This scale has a range of total scores from 0-90. A higher score indicates higher self-efficacy for exercise. The internal consistency has been reported as 0.92. When considering validity, the mental and physical health scores on the SF-12 questionnaire predicted efficacy expectations as measured by the SEE Scale. Furthermore, SEE efficacy expectations predicted exercise participation.
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Not Confident | Very Confident | |||||||||
| How confident are you right now that you could exercise three times per week for 20 minutes if: | ||
|---|---|---|
| Item | Context | Score |
| 1 | The weather was bothering you | |
| 2 | You were bored by the program or activity | |
| 3 | You felt pain when exercising | |
| 4 | You had to exercise alone | |
| 5 | You did not enjoy it | |
| 6 | You were too busy with other activities | |
| 7 | You felt tired | |
| 8 | You felt stressed | |
| 9 | You felt depressed | |
| SEE Total | ||
Exercise Benefits/Barriers Scale
Below are statements that relate to ideas about exercise. Please indicate the degree to which you agree or disagree with the statements by circling SA for strongly agree, A for agree, D for disagree or SD for strongly disagree (Sechrist et al., 1987).
| Item | SA | A | D | SD |
|---|---|---|---|---|
| 1. I enjoy exercise | ||||
| 2. Exercise decreases feelings of stress and tension for me | ||||
| 3. Exercise improves my mental health | ||||
| 4. Exercising takes too much of my time | ||||
| 5. I will prevent heart attacks by exercising | ||||
| 6. Exercise tires me | ||||
| 7. Exercise increases my muscle strength | ||||
| 8. Exercise gives me a sense of personal accomplishment | ||||
| 9. Places for me to exercise are too far away | ||||
| 10. Exercising makes me feel relaxed | ||||
| 11. Exercising lets me have contact with friends and persons I enjoy | ||||
| 12. I am too embarrassed to exercise | ||||
| 13. Exercising will keep me from having high blood pressure | ||||
| 14. It costs too much money to exercise | ||||
| 15. Exercising increases my level of physical fitness | ||||
| 16. Exercise facilities do not have convenient schedules for me | ||||
| 17. My muscle tone is improved with exercise | ||||
| 18. Exercising improves functioning of my cardiovascular system | ||||
| 19. I am fatigued by exercise | ||||
| 20. I have improved feelings of wellbeing from exercise | ||||
| 21. My spouse (or significant other) does not encourage exercising | ||||
| 22. Exercise increases my stamina | ||||
| 23. Exercise improves my flexibility | ||||
| 24. Exercise takes too much time from family relationships | ||||
| 25. My disposition is improved by exercise | ||||
| 26. Exercising helps me sleep better at night | ||||
| 27. I will live longer if I exercise | ||||
| 28. I think people in exercise clothes look funny | ||||
| 29. Exercise helps me decrease fatigue | ||||
| 30. Exercising is a good way for me to meet new people | ||||
| 31. My physical endurance is improved by exercising | ||||
| 32. Exercising improves my self-concept | ||||
| 33. My family members do not encourage me to exercise | ||||
| 34. Exercising increases my mental alertness | ||||
| 35. Exercise allows me to carry out normal activities without becoming tired | ||||
| 36. Exercise improves the quality of my work | ||||
| 37. Exercise takes too much time from my family responsibilities | ||||
| 38. Exercise is good entertainment for me | ||||
| 39. Exercising increases my acceptance by others | ||||
| 40. Exercise is hard work for me | ||||
| 41. Exercise improves overall body functioning for me | ||||
| 42. There are too few places for me to exercise | ||||
| 43. Exercise improves the way my body looks |
Simple Benefits/Barriers Assessment
| What do you see as the benefits of exercise? | |
| 1. | |
| 2. | |
| 3. | |
| What do you see as being barriers to exercise? | |
| 1. | |
| 2. | |
| 3. | |
Lab Question 3
| From your perspective, what are the five greatest barriers to exercise participation? | |
| 1. | |
| 2. | |
| 3. | |
| 4. | |
| 5. | |
Exercise Adherence Assessments
Many functional status questionnaires are completed prior to and following an exercise intervention in order to examine any changes that may have occurred as a result of the training period. Naturally, it is important to concurrently report the participant’s compliance to the program to ensure that any changes were due to this intervention rather than any extraneous variables.
Participant compliance to a program may be calculated using a simple formula:
Compliance = Number of sessions completed / Number of sessions available
There are several methods of assessing program compliance, however, the level of scrutiny depends on the required level of enquiry. Some researchers/practitioners only need information about the number of sessions that the client has performed, whereas others require more detailed information about session intensity, duration and rate of progression. In most circumstances, it is best to develop a questionnaire based on the needs of the client.
Additionally, the term ‘adherence’ better encapsulates a more holistic buy-in from the participant. An individual who adheres to the program has input to the weekly activities, is involved with setting goals, and tends to have a level of involvement that requires a qualitative set of measures to assess. Please consider the similarities between compliance and adherence when implementing the formula to compute either variable.
Lab Question 4
| List four possible methods to improve exercise adherence for a group of three friends - asthmatic, young adult females - who started an exercise program in a group as a new year’s resolution. Their current adherence rate is 50-60%. They commenced the program in an attempt to lose weight and improve their breathing function so they did not feel so out of breath as often throughout the day. They meet at the local park on 4 mornings per week and perform a variety of ‘bootcamp’ style exercises under the watchful eye of a personal trainer. |
|
| 1. | |
| 2. | |
| 3. | |
| 4. | |
References
Lab Session - Part B
Accuracy of Daily Activity Monitors
Introduction
Physical inactivity is a primary cause of the major metabolic diseases. Whilst there are many confounding factors that contribute to these diseases, including genetics, dyslipidaemia and cardiovascular disease, sedentary behaviour is perhaps the primary cause of obesity and impaired insulin sensitivity. With the introduction of physical activity into daily life, individuals with metabolic diseases can significantly reduce the risk of mortality and improve their quality of life.
Physical activity is a proven method of achieving and maintaining a negative energy balance (to attain an ideal body mass). Monitoring physical activity is important in two main ways:
Physical activity measures are used diagnostically to assess current physical activity patterns.
Physical activity measures are used as a prescriptive tool, with a target distance to cover/number of steps per session being prescribed. In this way, the pedometer can also act as an incentive for participants to cover a set amount of work in a day.
It is common for practitioners to prescribe physical activity to clients with metabolic diseases, however, this activity must be prescribed on an individual basis. Current physical activity status, aerobic fitness, exertional distress and any injuries must be considered when prescribing an exercise program. For monitoring purposes, daily activity logs are often compiled by patients/clients, however, inaccurate responses are very common among patients with obesity and other metabolic diseases. Equipment such as pedometers, accelerometers and global positioning system (GPS) units provide objective measures of the amount of activity performed on any given day, and are accordingly far more reliable than other recording methods.
The objectives of this lab activity are to:
- Gain experience using standard items to assess daily physical activity
- Examine the effectiveness of using physical activity monitors
Methods
Equipment
GPS monitor
2 x Pedometers (1 x basic unit; 1 x phone-based unit)
Measuring tape or trundle wheel
Pedometers
Pedometers are electronic devices that are used to measure the number of steps taken over a given time period. Usually worn at the hips, the quality of measurement varies between units, however, these counters can provide valuable information regarding movement patterns. Generally, pedometers are used to monitor or prescribe the number of steps for an individual, rather than directly attempting to quantify distance. However, there may be merit in attempting to obtain distance data from these units, as step length can be used to calculate distance.
When considering daily step counts, the following guidelines represent different activity classes:
Fewer than 5,000 steps per day = sedentary
5,000–7,499 = low active
7,500–10,000 = somewhat active
10,000–12,499 = active
12,500+ steps per day = highly active
Due to individual differences in metabolic rate and intensity of walking, it is difficult to calculate energy expenditure from number of steps taken per day. However, energy expenditure may be approximated from the data obtained, with a greater number of steps correlating with a greater energy expenditure.
Some pedometers allow the entry of physical data such as height, body mass, or other characteristics to provide a more accurate estimate of energy expenditure. Whilst providing a guide to energy expenditure, these measures need to be treated with caution due to their lack of direct physiological measurement.
A large scale research project incorporating physical activity prescription using pedometers is the 10,000 steps program based in Rockhampton, QLD. The project has attempted to increase physical activity in a regional town in an attempt to offset the growing obesity crisis. Participants are encouraged to wear a pedometer and undertake a minimum of 10,000 steps per day, through either incidental exercise during the day, or formal sport/exercise participation. In an attempt to maximise adherence, support is available to participants via phone calls and online resources. Researchers have determined that this quantity of physical activity (10,000 steps) approximates the guidelines for general health, although a greater number of steps per day is encouraged.
For more information about this program, go to 10000steps.org.au. In January 2025, they report that 685,547 members have logged a grand total of 432,606,819,172 steps! Similar gamification or reward models exist, for example Qantas Wellbeing.
Accelerometers
Accelerometers can provide a better measure of activity compared to pedometers as they can distinguish between walking, running, and even more explosive movements (e.g., jumping). Rather than a binary outcome offered by a pedometer (step or no step), accelerometers offer information about the magnitude/intensity of movement. Complex algorithms can also separate movement derived from skeletal muscle force output and movement generated outside the human capability, such as that recorded from riding in a car. Due to their precision and reliability, accelerometers are often used to validate pedometer step counts and are, therefore, a gold standard method for measuring physical activity.
Accelerometers operate by measuring acceleration along a given axis. They are typically tri-axial (i.e., coronal, vertical, and anteroposterior), enabling measurement of movement in multiple planes (frontal, sagittal, and transverse). Mechanistically, the accelerometer sensor converts movements into electrical signals (counts) that are proportional to the muscular force responsible for producing motion (Melanson & Freedson, 1996). These counts are summed over a specified period of time and stored. This period is often 24 hours, or can be up to 2-3 full months depending on battery and storage capacity. Segmenting accelerometer data enables the determination of activity patterns which leads to deeper analyses, e.g., sleep vs awake time, and can provide information about temporal patterns of exercise.
For a review of this technology see Yang & Hsu (2010). A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors, 10(8): 7772-7788. doi.org/10.3390/s100807772
GPS monitors
GPS (Global Positioning System) technology has revolutionised the way that exercise scientists are able to track athletes and research subjects. Small GPS chips are very affordable and user-friendly, with many different models available for <$300. GPS units obtain position data from up to 31 currently-orbiting satellites that, with clear skies and an open area, can provide accurate location data to within 30 cm with modern mobile phones (typically closer to 5 m). Military and engineering applications can achieve sub-millimeter accuracy. Most GPS units measure position once per second (1 Hz), however some can log data at much higher frequencies, e.g., 5, 10, or 100 Hz, increasing accuracy (and file size).
Together with GPS data, most monitors also record heart rate to provide a more accurate measure of energy expenditure. This has obvious benefits for quantifying training loads and volumes. GPS monitors have been shown to accurately record distance and speed, however some factors can increase measurement error. Low measurement frequency can result in missed movements where faster movement patterns have greater error due to rapid changes in latitude/longitude. Additionally, the built and natural environment (buildings, trees, clouds) can also obstruct line-of-sight between the GPS unit and satellites. You may have noticed on your Strava map that the GPS trace sometimes goes wandering all over the road. This error can lead to overestimation of distance covered (about 5%). This represents a clear limitation of GPS-based tracking, which makes it unsuitable in some scenarios. Indoor positioning systems have been developed with very high accuracy (2 cm), which may make this less of a limitation (Serpiello et al., 2018; Spinney et al., 2015).
When considering the use of GPS for tracking of humans, a pioneering article by Duncan et al. (2007) stated that:
GPS measures position, distance, and speed based on the time taken to receive a signal from orbiting satellites; manufacturers report commercially available GPS to be accurate to within 15 m. High levels of precision were demonstrated by Wide Area Augmentation System (WAAS)-enabled Garmin GPS (Garmin Ltd., Olathe, KS) while the unit was stationary, with 99% of all points falling within 20 m of the actual location. GPS also recently has been used to assess a variety of human activities, making GPS an attractive alternative to self-report and other objective measures currently available to assess active transport travel distance, although this is largely unstudied. Previous research has demonstrated that physical activity can be assessed without substantial changes to behaviour attributable to the measurement process or measurement reactivity; therefore, GPS also may be used to assess active transport without bias introduced by measurement reactivity. Given the importance of distance as a barrier to active transport, it is imperative to gain accurate measures of distance travelled, to understand how the likelihood of active transport engagement varies by distance.
Despite being more than a decade old, the paper highlights the potential use of GPS tracking when assessing daily physical activity. Participants are more likely to undertake their standard levels of movement as the devices are unobtrusive, and individuals may even develop a sense of forgetting that they are being monitored. Sensor technology improves each year, with high precision sensors being standard features in smart watches and phones. Common GPS units used in sport are from Catapult Sports (catapultsports.com) and Garmin (garmin.com).
The reliability of pedometers and GPS monitors have been published previously. In today’s lab session, we will be considering their accuracy relative to a criterion measure, with a view to considering their use in exercise prescription.
Procedure
- Set up subject with GPS unit and 2 x pedometers.
- The subject is required to perform the following:
- 1 lap of the field at a slow walking speed
- 1 lap of the field at a fast walking speed
- 1 lap of the field running
- Measure the number of steps from each of the pedometers and calculate approximate distance for each activity. Record the distance from the GPS unit for each activity. Reset each unit after each trial.
- Calculate the percentage difference between the criterion measure and the pedometers and GPS units.
Results
Calculate the percentage differences between the criterion measure (actual steps or actual metres) and each of the other measurement units.
To calculate the percentage difference you need to use the following formula:
%diff = (device measurement - actual measurement) / actual measurement × 100
| Percentage difference | Slow Walk | Fast Walk | Running |
|---|---|---|---|
| 1. Cheap Pedometer-reported steps vs Actual steps | |||
| 2. Phone Pedometer-reported steps vs Actual steps | |||
| 3. Cheap Pedometer distance vs Actual distance | |||
| 4. Phone Pedometer distance vs Actual distance | |||
| 5. GPS distance vs Actual distance | |||
| 6. Cheap Pedometer vs Phone Pedometer steps |
Discussion
Does the data support the use of pedometers in approximating distance covered on a daily basis?
Explain why pedometers are considered to be useful for general health.
Is the level of error produced by the GPS monitor acceptable? What recommendations would you make to improve the quality of the data? Would you recommend the use of a GPS monitor in the determination of distance covered on a daily basis? Why or why not?
Discuss the role of physical activity in the:
- Prevention of cardiopulmonary and metabolic conditions?
- Discuss the role of physical activity in the treatment of cardiopulmonary and metabolic conditions.
Prescribe a training program for an obese individual with type 2 diabetes who is looking to lose ~20kg over a 10 month period? Explain distances, intensity, modality, frequency etc. Would you encourage the use of a pedometer or GPS unit? If so, in what way would it be included?
Now consider what programming variables would be different for prescribing exercise for individuals with arthritis or osteoporosis. Would you encourage the use of a pedometer or GPS unit? If so, in what way would it be included?
If you are using the online lab manual, when you have completed the lab content and discussion questions for this week, print this webpage to PDF to save a copy on your device
All text entry boxes will clear if you leave or refresh this page
References
Part A
American College of Sports Medicine (2017). ACSM’s Guidelines for exercise testing and prescription, 10th edn. Lippincott Williams and Wilkins: Philadelphia.
Godin, G. (2011). The Godin-Shephard leisure time physical activity questionnaire. Health & Fitness Journal of Canada. 4(1): 18-22.
Hltaky, M.A., Boineau, R.E. et al. (1989). A brief self-administered questionnaire to determine functional capacity (The Duke Activity Status Index). American Journal of Cardiology. 64: 651-654.
Powell, L.E. & Myers, A.M. (1995). The Activities-specific Balance Confidence (ABC) Scale. Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 50(1): M28-M34.
Resnick, B., & Jenkins, L. S. (2000). Testing the Reliability and Validity of the Self-Efficacy for Exercise Scale. Nursing Research, 49: 154-159.
Sechrist, K.R., Walker, S.N. & Pender, N.J. (1987). Development and psychometric evaluation of the Exercise Benefits/Barriers Scale. Research in Nursing and Health, 10: 357-365.
Part B
Duncan, M. J., Mummery, W. K. & Dascombe, B. J. (2007). Utility of Global Positioning System to Measure Active Transport in Urban Areas. Med Sci Sports Exerc. 39(10): 1851–1857.
Melanson Jr. E.L., Freedson, P.S. & Blair, S. (1996). Physical activity assessment: A review of methods. Crit Rev Food Sci Nutr. 36: 385-396.
Serpiello, F. Hopkins, W. Barnes, S., Tavrou, J., Duthie, G., Aughey, R. & Ball, K. (2018) Validity of an ultra-wideband local positioning system to measure locomotion in indoor sports. Journal of Sports Sciences, 36(15): 1727-1733.
Spinney, R., Smith, L., Ucci, M., Fisher, A., Konstantatou, M., Sawyer, A., Wardle, J. & Marmot, A. (2015). Indoor Tracking to Understand Physical Activity and Sedentary Behaviour: Exploratory Study in UK Office Buildings, PLoS ONE, 10(5): e0127688.
Wieters KM, Kim JH & Lee C. (2012). Assessment of wearable global positioning system units for physical activity research. Journal of Physical Activity and Health. 9(7):913-23.
Yang, C-C & Hsu, Y-L (2010). A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors, 10(8): 7772-7788.